Abstract
Background:
Venous thromboembolism (VTE) has an estimated incidence of 1-2 per 1000. Despite anticoagulation, many patients suffer from its complications: VTE recurrence rate after an unprovoked VTE is 30%, and the rate of post-thrombotic syndrome is 25-50%. Statins are commonly used for cardiovascular diseases, and their anti-inflammatory properties have been shown to improve clot resolution in mouse models. Therefore, it could be a potential adjunct therapy for acute VTE to expedite clot resolution and reduce morbidities. Here we report initial data of a randomized open label study to investigate the effect of statins on biomarkers and clinical outcomes in patients with acute VTE.
Objectives:
To evaluate the effect of atorvastatin on thrombin generation, biomarkers and clinical outcomes in patients with acute VTE receiving anticoagulation. We hypothesize that the addition of atorvastatin can reduce thrombin generation and inflammation.
Patients/Methods:
Adult patients with newly diagnosed acute proximal acute proximal deep vein thrombosis (DVT) +/- pulmonary embolism (PE) were enrolled and randomized 1:1 to standard of care (SOC) (anticoagulation), or SOC plus atorvastatin 40 mg daily. Patients were enrolled within 21 days an acute VTE diagnosis. Fasting blood samples were drawn on enrollment, 3 months, and 9 months, for routine blood tests, thrombin generation, selective cytokines and lipidomic profiles. Clinical outcomes were monitored, including recurrent venous or arterial thromboses, major bleeding events, and post thrombotic symptoms evaluated by the Villalta score. Patients were excluded if they received thrombolysis or statins within 6 weeks prior to enrollment, had malignancy diagnosed within 2 years, pregnant or lactating. Thrombin generation assays were performed using a commercial kit (TECHNOTHROMBIN® TGA, Technoclone, Vienna, Austria) according to the manufacturer's instructions. Parameters recorded included peak thrombin concentration and endogenous thrombin potential (ETP). Two sample t-test were used to compare the differences of two arms with alpha of 0.05.
Results:
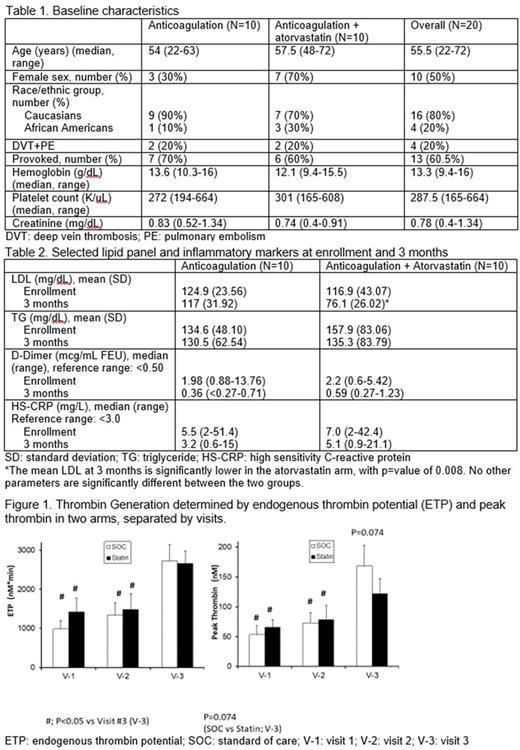
From February 2015 to June 2017, twenty patients were enrolled. Ten were randomized to each arm, SOC vs SOC+statin. The baseline characteristics are summarized in Table 1. The median age is 55.5 years, 50% are female, and 80% are Caucasians. All patients had proximal lower extremity DVT, while 4 (20%) had concurrent PE. All patients have completed 3 month follow-up and 17 (85%) have completed 9 month visits. Eleven patients (55%) were treated with warfarin, the remainder with rivaroxaban. Duration of anticoagulation was at the discretion of the treating physician, with seven patients (35%) continuing on anticoagulation at the most recent visit, resulting in a median duration of anticoagulation to be 6.1 (range 3.3-11.1) months. Two patients were lost to follow-up after the 3 month visit, and two refused the 9-month blood draw. No patients had recurrent VTE or major bleeding on study. Seven (70%) patients on SOC arm compared to 8 (80%) on SOC+statin arm had residual chronic DVT noted on ultrasound at 3 months. The median Villalta score for the affected extremity on enrollment for each arm was 5.5 vs 4.5 (SOC vs SOC+statin), and 4.5 vs 3.5 at 3 months. The mean LDL at 3 months is significantly reduced in patients on statin arm compared to SOC arm, while other markers are not different (Table 2).
Figure 1 shows the differences between SOC and SOC+statin by ETP and peak thrombin, separated by visits. There are no significant differences between SOC and SCO+statin arms (Figure 1). Patients have higher thrombin peak and ETP at visit 3 (9 month visit) in both arms, which may be explained by 8 of 13 patients being off anticoagulation at visit 3. When analysis is done based on anticoagulation status at visit 3, reduced peak thrombin and ETP are found in patients on anticoagulation compared to those who are not.
Conclusions:
In this small pilot study, atorvastatin 40 mg daily did not reduce thrombin generation at 9 months, when used in combination with standard anticoagulation as treatment for an acute VTE. At present the study is limited by the small sample size due to slow recruitment. Atorvastatin did reduce LDL, and may alter inflammatory states, and further analyses of inflammatory markers and lipidomic are ongoing to evaluate the effect of atorvastatin on VTE-related inflammation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal